2018-2023 Report
Our team was established in 2024-2025 and brings together members from former teams within the center, who already shared a common interest in studying the reciprocal interactions between mental and brain disorders and the environment of affected individuals. This research is conducted through the analysis of affective, cognitive, and social processes. The work carried out during the previous mandate (2018-2023) has been synthesized into three main research areas:
A first series of studies focused on the visuo-perceptual deficits observed in individuals with severe alcohol use disorder (SAUD) to determine whether these deficits could, at least in part, explain the higher-level cognitive difficulties observed in these patients, particularly in the processing of emotional information (Creupelandt et al., 2019). Our research suggests that these visuo-perceptual alterations originate as early as the initial stages of sensory processing (Creupelandt, D’Hondt et al., 2021; Creupelandt, Maurage, and D’Hondt, 2021), possibly at the retinal level (Creupelandt, Maurage, Lenoble et al., 2021), affecting both magnocellular and parvocellular processing (Creupelandt, D’Hondt et al., 2022; Creupelandt, Maurage et al., 2022). These early processing anomalies may profoundly impact cognitive processes, particularly the decoding of emotional facial expressions (Creupelandt et al., 2020). The extent of these impacts can vary within the SAUD population (Maurage, Pabst et al., 2021), aligning with the heterogeneity observed in cognitive deficits (D’Hondt et al., 2018). Recognizing this heterogeneity is crucial for developing therapeutic strategies (Rolland et al., 2019), particularly in the implementation of cognitive remediation (Maurage et al., 2023).
A significant part of our work has focused on examining attentional processes and biases toward affective information, which are frequently observed in mental disorders. In particular, we have used eye-tracking to study the mechanisms by which individuals prioritize, engage with, and sustain attention on emotional stimuli compared to neutral stimuli.
As part of our collaboration with UCLouvain, we have conducted a series of eye-tracking studies, building on previous research demonstrating the value of this technique in exploring alcohol use disorders (Maurage, Masson et al., 2020; Maurage, Bollen et al., 2020, 2021). These studies specifically examined the mechanisms underlying attentional biases toward alcohol-related cues (Bollen, D’Hondt et al., 2021). Our findings showed that binge drinkers direct more attention toward these cues when their craving level is high (Bollen et al., 2020), whereas individuals in recovery from severe alcohol use disorder (SAUD) tend to avoid these cues, potentially reflecting their intention to maintain abstinence (Bollen, Pabst et al., 2021).
Meanwhile, our research conducted in Lille highlighted a general tendency to allocate more attentional resources to negative stimuli than to simultaneously present neutral stimuli (Veerapa et al., 2020). This phenomenon is exacerbated in patients with post-traumatic stress disorder (PTSD), where the bias toward negative information intensifies with prolonged exposure to stimuli (Veerapa et al., 2023). These results support cognitive theories of PTSD, emphasizing the central role of biased processing of negative information and advocating for targeted interventions to reduce these biases.
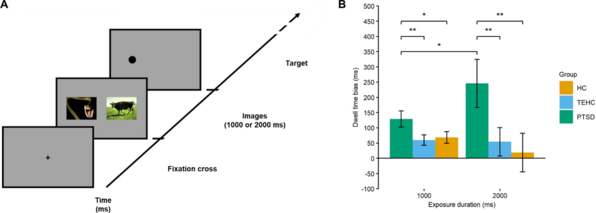
(A) Dot-probe task. A trial is triggered when fixation on the central cross is stable for 500 ms. Each trial begins with a black fixation cross presented on a gray background for a randomly selected duration between 500 and 1,500 ms, followed by two stimuli—a neutral scene and a negative scene—simultaneously displayed for either 1,000 ms or 2,000 ms. A small black dot then appears randomly in the location previously occupied by either the negative image (congruent trials) or the neutral image (incongruent trials). Participants must first fixate on the central cross, freely explore the images, and then indicate as quickly as possible the spatial position (left or right) of the dot by pressing one of two keys.
(B) Mean fixation duration as a function of image exposure duration (1,000 or 2,000 ms) and group. Positive values indicate longer fixation on negative images compared to neutral images. HC, healthy control subjects; PTSD, post-traumatic stress disorder; TEHC, trauma-exposed healthy controls. Error bars represent the standard error of the mean (Morey, 2008). * p < 0.05, ** p < 0.01, *** p < 0.001. Adapted from Veerapa et al. (2023).
Finally, in a series of studies conducted in collaboration with the University of Mons, we used electroencephalography (EEG) to decode the attentional responses of children with high social anxiety when faced with social threats. Although no clear behavioral differences were observed, our analyses revealed distinct neural processing patterns, suggesting a deeper attentional anchoring toward social threats in these children (Wauthia, Rossignol et al., 2022). These findings are associated with disengagement difficulties, likely linked to impairments in cognitive control (Wauthia, D’Hondt et al., 2022). This research opens new perspectives for developing targeted interventions aimed at addressing these specific neural mechanisms, with the potential to improve therapeutic outcomes for this vulnerable population.
A significant part of our research focuses on the underlying mechanisms of emotional experience and regulation in mental health disorders. We study affective processes and their neurobiological foundations to better understand individuals' emotional responses and their coping strategies.
We have been particularly interested in the FKBP5 gene, known for its crucial role in stress physiology and the modulation of the hypothalamic-pituitary-adrenal (HPA) axis (Amad, Ramoz et al., 2019). Our studies have shown that FKBP5 polymorphisms, frequently found in individuals with borderline personality disorder (BPD), are significantly associated with this disorder, highlighting the gene’s modulation by childhood trauma. Further exploring the shared neurobiological mechanisms between BPD and post-traumatic stress disorder (PTSD), our meta-analysis identified consistent patterns of reduced brain activation in the precuneus for both disorders (Amad, Radua et al., 2019). Additionally, specific alterations in the anterior cingulate cortex and superior frontal gyrus suggest distinct impairments in stress responses and emotional reactivity between these conditions.
Moreover, we have developed a new virtual reality-based paradigm to assess patients' emotional experiences, allowing us to compare their anticipated affective responses to future events with their actual emotional experiences when facing them. The ability to anticipate emotional responses to future events is a critical skill that influences decision-making and behavioral orientation. Our initial application of this virtual reality paradigm highlighted significant biases in affective forecasting, demonstrating that individuals often anticipate more intense emotional reactions than they actually experience during the event (Loisel-Fleuriot et al., 2023). Our study further revealed a link between anticipated responses and electrodermal activity recorded during anticipation, mirroring the physiological responses observed during emotion induction in external environments. These findings offer promising avenues for studying psychiatric populations characterized by anxious anticipation, as well as addictive populations, where deficits in anticipating the negative consequences of consumption behaviors appear to be a key issue.
Over the past two decades, clinical tests designed to assess social cognition and affective processing abilities have emerged. This field has proven essential in guiding differential diagnoses across various clinical conditions. For instance, in neurodegenerative disease research, we and others have demonstrated the usefulness of these measures in distinguishing neurologically similar disorders such as Alzheimer’s disease (AD) and frontotemporal degeneration (FTD). Social cognition is particularly relevant, as recent findings show that other domains previously considered useful for differential diagnosis are, in fact, uninformative. For example, we observed that memory impairments are not as predictive of Alzheimer’s pathology as previously thought, failing to differentiate AD from FTD at initial presentation (Bertoux et al., 2020), as both diseases involve similar brain regions, such as the hippocampal and perihippocampal areas (Bertoux et al., 2018).
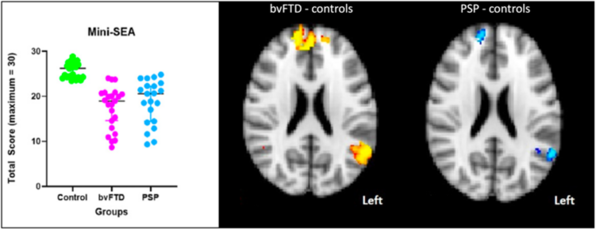
To date, research has primarily focused on the cognitive variants of neurodegenerative diseases. It remains unclear whether social cognition is preserved in other neurodegenerative disorders where motor symptoms typically overshadow cognitive difficulties, such as progressive supranuclear palsy (PSP), a motor variant of FTD, or Parkinson’s disease. We conducted cognitive and neuroimaging comparisons between AD, the behavioral variant of FTD (bvFTD), PSP, and Parkinson’s disease and explored correlations between social cognition performance and brain imaging. We observed significant deficits in mentalization and emotion recognition in PSP, correlated with atrophy in frontal, cingulate, insular, and limbic regions. Overall, the cognitive and imaging profiles of PSP were similar to those observed in bvFTD (Bertoux, de Souza et al., 2022). Comparing AD, bvFTD, and Parkinson’s disease, we found that social cognition measures were the most reliable indicator for differentiating bvFTD from Parkinson’s disease, achieving an accuracy of 98.3%. Combined with a simple cognitive screening measure, social cognition also effectively distinguished bvFTD from AD and AD from Parkinson’s disease with high precision (Ibanez et al., 2021). Specific patterns of atrophy and functional networks across neurodegenerative diseases have been linked to social cognition performance.
Social cognition has also been considered a promising domain for distinguishing bvFTD from atypical late-onset psychiatric disorders, a context that remains a clinical challenge. More than 50% of bvFTD patients are misdiagnosed with psychiatric disorders, leading to delays in appropriate care. This aligns with our findings from an analysis of 690 bvFTD cases and 18,831 AD cases within our regional memory clinic network (Leroy, Bertoux et al., 2021). To address this issue, we initiated a new line of research to conduct in-depth comparisons between bvFTD patients and those with late-onset psychiatric disorders. Following our initial study comparing bvFTD patients with those suffering from major depressive disorder (Bertoux et al., 2012), we extended our investigations to patients with bipolar disorder. Our findings indicated that, at least quantitatively, social cognition performance alone did not distinguish between these patient groups (Barbosa et al., 2023). These preliminary results have paved the way for further projects aimed at conducting comprehensive comparisons of clinical, cognitive (including qualitative analyses), and neuroimaging domains between bvFTD patients and those with late-onset psychiatric disorders.
Although this remains a topic of debate in the literature, social cognition is often considered a distinct domain, relatively independent from other cognitive functions. Additionally, its assessment is typically focused on a key-process-centered approach, taking into account only mentalization (or theory of mind) and facial emotion recognition. We argue that, while essential for drawing attention to this often-overlooked domain, such perspectives may hinder a comprehensive understanding of human cognitive architecture and a precise analysis of social behavior. Therefore, we have proposed two hypotheses: (i) mentalization and emotion recognition alone are insufficient to capture the complexity of social cognitive abilities, and other often-neglected mechanisms should be considered; (ii) since social behavior cannot result from a single isolated cognitive mechanism, cognitive phenomena should not be studied in isolation. Cognitive interactions should be taken into account when exploring synergistic processes such as social interactions (Quesque et al., 2022a).
To illustrate the first hypothesis, we conducted a single-case study with a patient diagnosed with Klüver-Bucy syndrome. Our findings showed that traditional neuropsychological assessments were weakly correlated with social adaptation difficulties, providing little insight into severe reversal learning impairments related to social cognition and affective processing following brain damage (Bertoux et al., 2018). We also found that other cognitive processes, such as reversal learning, decision-making, and creative thinking, may also be relevant in this context, alongside mentalization and emotion recognition.
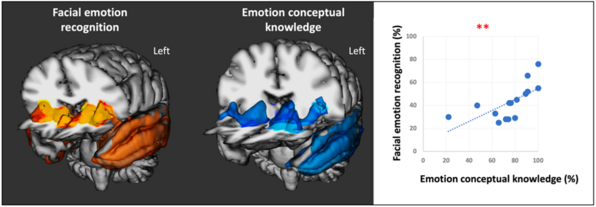
Subsequent studies addressed both hypotheses. We used neurodegenerative diseases as lesion models to examine key cognitive dysfunctions and their impact on other cognitive abilities. Our findings challenged the traditional view of cognitive abilities as compartmentalized and isolated, instead demonstrating that they are interwoven and interdependent. For instance, we explored environmental dependency syndrome, typically attributed to compulsive object manipulation due to executive dysfunction following frontal lobe damage. In a study with patients suffering from the behavioral variant of FTD (bvFTD), this syndrome was predicted by both mentalization difficulties and executive impairments, suggesting that in contexts where patients struggle to understand the expected action from a clinician, environmental cues may be exploited to guide behavior (Flanagan et al., 2018). In another study on emotion processing in the semantic variant of FTD, we found that difficulties in recognizing facial emotions were strongly correlated with the loss of conceptual knowledge associated with those emotions. This was further reflected in significant involvement of brain regions related to affect and semantics, providing novel clinical evidence supporting constructivist theories of emotions (Bertoux et al., 2020).
In collaboration with the University of Cambridge (United Kingdom), the Brain & Mind Centre at the University of Sydney (Australia), and the École Normale Supérieure (Paris, France), we employed a neuroeconomic paradigm to highlight the role of affective processing in economic decision-making tasks. This was achieved by identifying affective biases in a population with lesions in the ventromedial prefrontal cortex (Lenglin et al., 2023). Additionally, we examined the relationship between interoceptive accuracy and the ability to infer mental states in chronic pain disorders, hypothesizing a common inferential mechanism based on the brain's predictive coding model. While we observed reduced interoceptive accuracy and impaired mentalization performance in patients with chronic lower back pain, no correlation was found between these capacities (El Grabli et al., 2022).
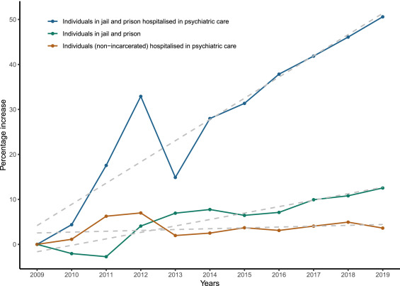
This line of research aims to better understand the specific mental health challenges faced by incarcerated individuals. Our studies reveal a concerning prevalence of psychiatric disorders and substance use disorders among newly incarcerated individuals in France (Fovet et al., 2020). In particular, we have highlighted that psychotic disorders are especially frequent among incarcerated men (Fovet, Pignon, Wathelet et al., 2023). While incarceration can exacerbate these disorders, individual and socio-environmental vulnerability factors also play a major role, calling for a more nuanced understanding of psychotic manifestations in this high-stress context (Fovet, Wathelet, Pignon et al., 2022).
Furthermore, our research indicates that incarceration is a risk factor for dual pathology, characterized by the co-occurrence of a psychiatric disorder and a substance use disorder (Fovet, Wathelet, Benbouriche et al., 2022). We also emphasize the importance of direct comparisons between the incarcerated population and the general population (Fovet, Wathelet, Amad et al., 2023). These comparative analyses highlight the increased vulnerability of incarcerated individuals to post-traumatic stress disorder (PTSD) and its associated comorbidities.
Finally, we have evaluated the impact of the creation of psychiatric hospital units dedicated to incarcerated individuals. While these structures play a key role, significant barriers to hospitalization access remain, underscoring the structural challenges of psychiatric care in correctional settings (Fovet, Chan-Chee et al., 2022).
The COVID-19 pandemic created an exceptionally stressful context, marked by prolonged social isolation and major constraints on interpersonal relationships. From the onset of the crisis, our team, in close collaboration with the Cn2r, mobilized to assess its impact on mental health, with a particular focus on post-traumatic stress disorder (PTSD).
Our pioneering studies in France revealed a 6.5% prevalence of PTSD among patients hospitalized for COVID-19 (Horn et al., 2020) and an almost twofold lower rate among older individuals (Horn et al., 2022). These findings align with previous research suggesting greater resilience in older adults in non-COVID-19-related traumatic contexts. We also highlighted the critical role of liaison psychiatry, demonstrating the increased risk of functional somatic disorder (FSD) linked to the direct effects of the virus, hospitalization stress, and treatment side effects, exacerbated by fear and uncertainty surrounding the illness (Horn et al., 2021). Our study found that approximately 10% of patients in our Lille cohort diagnosed with COVID-19 exhibited FSD, with a significant association between its severity and a probable PTSD diagnosis (Horn et al., 2023).
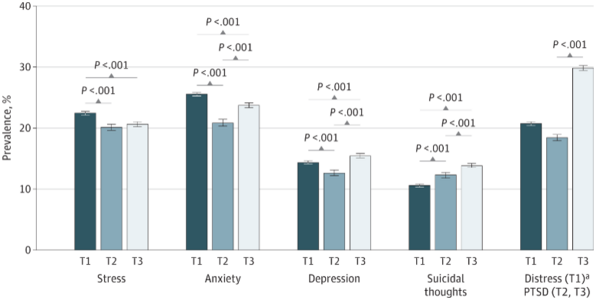
The pandemic also reignited debates on the nosology of PTSD, particularly concerning the definition of a traumatic event and whether the pandemic and associated health measures could be considered traumatic (Wathelet, D’Hondt, et al., 2021). Our COSAMe survey of university students, one of the largest global samples on this topic, revealed alarming levels of distress in this vulnerable population (Wathelet et al., 2020). During the first lockdown, 22.4% of students (N = 69,054; T1) reported acute stress (Wathelet et al., 2020). Additionally, our data indicated a significant increase in PTSD prevalence over time, rising from 19.5% (N = 22,883; T2) one month after the first lockdown ended (Wathelet, Fovet, et al., 2021) to 31.0% (N = 44,898; T3) 15 months later (Wathelet et al., 2022).
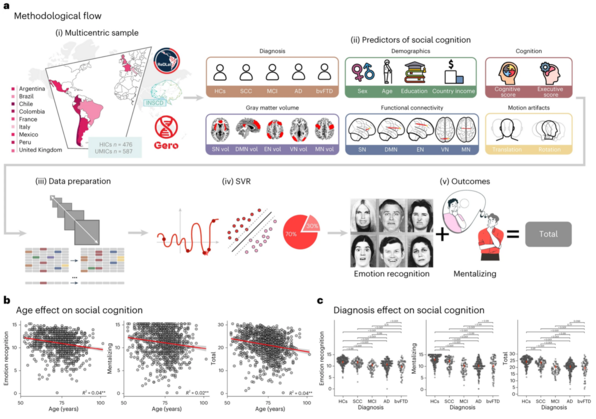
Now recognized as essential in the field of mental health, social cognition measures are increasingly used to quantify symptoms, assess therapeutic interventions, and guide clinical diagnoses. However, the applicability of traditional social cognition measures, primarily developed in WEIRD (Western-Educated Industrialized Rich Democratic) countries, has not yet been thoroughly explored in truly cross-cultural contexts.
Over the past decade, cross-cultural comparisons have typically involved only two (or at most three) countries, usually an English-speaking country and an Asian country. In this context, we aimed to estimate the influence of nationality on standard social cognition measures. By coordinating a standardized neuropsychological assessment across 18 sites in 12 countries, we observed that beyond age and education, geographic differences accounted for the majority of the variance observed in facial emotion recognition and mentalization measures (Quesque et al., 2022b). These findings highlight the urgent need for the harmonization and cultural adaptation of neuropsychological tools for social cognition.
The results of our study have played a key role in launching several ongoing international initiatives aimed at harmonizing these measures across Europe and globally. Through two international collaborations, we have also demonstrated the importance of education as a key predictor of social cognition performance (de Souza et al., 2018; Fittipaldi et al., 2024). Overall, we believe these findings are crucial for promoting an ethical and informed understanding of social cognition, grounded in a more inclusive global perspective.
Catatonia, characterized by the abolition of interactions between individuals and their environment, is a complex psychomotor syndrome encompassing various motor, affective, and behavioral manifestations. Understanding its pathophysiology and treatment response, particularly through neuroimaging, has been a central focus of our team’s research. The primary objective has been to improve our ability to assess catatonia and optimize therapeutic interventions accordingly (Leroy et al., 2018).
Through extensive reviews and empirical studies, we have identified widespread brain imaging abnormalities associated with catatonia (Haroche et al., 2020) and confirmed the feasibility and utility of neuroimaging in routine clinical settings (Magnat et al., 2023). Furthermore, our research has highlighted the frequent co-occurrence of catatonia and dementia (Ramognino et al., 2024), shedding light on treatment resistance patterns and the need for tailored therapeutic approaches.
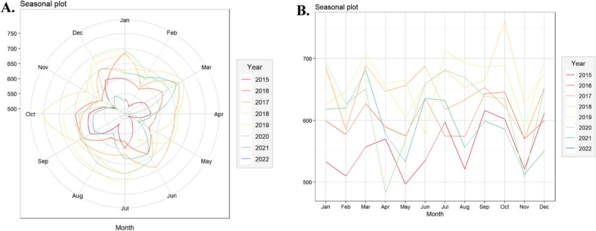
Using machine learning models and advanced statistical analyses, we have made progress in predicting treatment responses (Badinier et al., 2024) and identifying seasonal variations in catatonia diagnoses. These findings contribute to a deeper understanding of the complex nature of catatonia and guide the development of personalized interventions (Mastellari et al., 2024).
At the core of our approach is the application of diverse methods based on the theoretical concept of neuroplasticity. We have explored various aspects of plasticity, particularly its dependence on age, revealing how the timing of psychotraumatic events can critically influence their impact. This theme is further developed in our theoretical paper (Amad et al., 2020; see also Amad & Fovet, 2021), which integrates concepts from brain economy theories in collaboration with physicists.
Focusing on the therapeutic potential of neuroplasticity, we have critically analyzed the evolving discourse on the role of repetitive transcranial magnetic stimulation (rTMS) in treating neuropsychiatric disorders (Amad, Jardri et al., 2019), particularly depression. We examined its effectiveness within a context of varied evidence and diverse patient populations (Amad & Fovet, 2022). Our analyses emphasize the importance of situating rTMS within a nuanced therapeutic framework, advocating for its judicious application to improve the precision of mood disorder treatments. Furthermore, we highlight the necessity of distinguishing the therapeutic impact of rTMS from that of more established treatments such as electroconvulsive therapy (ECT), particularly in severe depressive episodes (Amad, Horn & Fovet, 2021). We advocate for rigorous, placebo-controlled methodological trials to confirm the role and efficacy of rTMS in treating major depressive disorder and treatment-resistant depression (Amad, Naudet & Fovet, 2019, 2023).
Expanding our research on neurocognitive stimulation, we have investigated the efficacy of transcranial direct current stimulation (tDCS) in two distinct contexts.
-
Dissociative Functional Epilepsy (DFE). We evaluated its potential as an intervention for this condition, known for its resistance to traditional pharmacological treatments. Our results showed significant reductions in seizure frequency, highlighting tDCS as a promising non-invasive therapeutic option (Leroy et al., 2024). A case study involving a 39-year-old woman also demonstrated success with PET-guided tDCS (Leroy et al., 2019). The protocol included tDCS sessions administered twice daily, five days a week, for three weeks. The results revealed a reduction in psychogenic involuntary movements and seizure frequency after five weeks of treatment, accompanied by improvements in PTSD symptoms, dissociation, depression, and alexithymia.
-
Binge drinkers. In collaboration with UCLouvain, we investigated the behavioral and electrophysiological effects of tDCS in mitigating cognitive impairments associated with binge drinking. This research demonstrated a specific improvement in the mobilization of attentional resources among binge drinkers, suggesting the potential of tDCS interventions for subclinical populations vulnerable to binge drinking-induced cognitive deficits (Dormal et al., 2020).
This body of research highlights the promise of neuromodulation as an innovative therapeutic lever and underscores the necessity of personalized and rigorous approaches to optimize its clinical impact.
The high incidence of suicide deaths within the first year following a non-fatal suicide attempt underscores the urgent need for vigilant prevention strategies during this critical period (Demesmaeker et al., 2022). Through brief contact interventions (BCI), our strategies prioritize the preservation of social connections as a central element in preventing suicidal relapse.
In particular, our team developed the ALGOS decision-making algorithm for suicide prevention, integrating various BCIs such as crisis cards, telephone follow-ups, and postcards aimed at reducing suicidal relapse among patients discharged after a suicide attempt (Vaiva et al., 2018). Analysis of the ALGOS study cohorts identified high-risk groups for suicide relapse or death within six months following an attempt, including individuals with alcohol use disorders, those who attempted suicide under acute alcohol influence, those with anxiety disorders, and those with multiple suicide attempts in the past three years (Demesmaeker et al., 2021a). A subsequent pharmaco-epidemiological study revealed an increased risk of relapse associated with the use of benzodiazepines and hypnotics, whether taken individually or in combination, within 14 months of a first attempt (Demesmaeker et al., 2021b).
Based on this research, the VigilanS program was implemented in the Hauts-de-France region before being expanded to other French regions. This program demonstrated a 38% reduction in suicide attempt recurrence compared to standard care (Santé Publique France, 2023). Data from VigilanS highlighted the need for intensified follow-up during the first months after a suicide attempt, particularly among men over 45 years old (Demesmaeker et al., 2023). The program is now being adapted for French correctional facilities to reduce suicide risk among incarcerated individuals. It focuses on its potential to mitigate feelings of isolation, a major risk factor for suicide in prison settings (Fovet, Wathelet, Jardon et al., 2023).